Treatment options for CAD
In the early stages, pharmaceutical treatment combined with changes in lifestyle and a healthy diet may be able to ease the symptoms and slow or even reverse the progress of CAD. If the disease is already advanced, the affected coronaries have to be widened mechanically. The cardiologist will recommend a combination of different treatment options based on the symptoms, the findings, and the future risks for the patient.
These options include
- Commitment to lifestyle changes
- Minimally invasive treatment: Percutaneous coronary intervention
- Balloon angioplasty
- Stenting
- Resorbable scaffold implantation
- Bypass surgery: coronary artery bypass graft
Medication and lifestyle changes
In patients with CAD, the cardiologist usually prescribes drugs to lower blood pressure in order to alleviate some of the heart’s workload. Those are typically beta-blockers, calcium channel blockers or diuretics. Aspirin and other antiplatelet agents prevent the blood from clotting; nitrates can quickly relieve chest pain; while statins may lower blood cholesterol. Since everyone is different, the cardiologist will develop a customized therapy plan for each patient.
In addition to pharmaceutical treatment, a healthy lifestyle is crucial to prevent or slow the worsening of the disease. Patients should quit smoking, exercise regularly and eat a diet low in fat and salt. For overweight patients, losing weight reduces the heart’s workload and lowers the risk of other disorders developing.
Percutaneous coronary intervention (PCI)
PCI (also called coronary angioplasty) is a treatment for CAD which can help improve the blood supply to your heart muscle by widening narrowed parts of a coronary artery. PCI uses a narrow flexible tube called a catheter. In the cath lab (a dedicated examination room in a hospital or clinic), the cardiologist accesses the blood system usually through the wrist or groin. Only tiny cut in the skin is needed to access the vessel.
Overview of PCI techniques
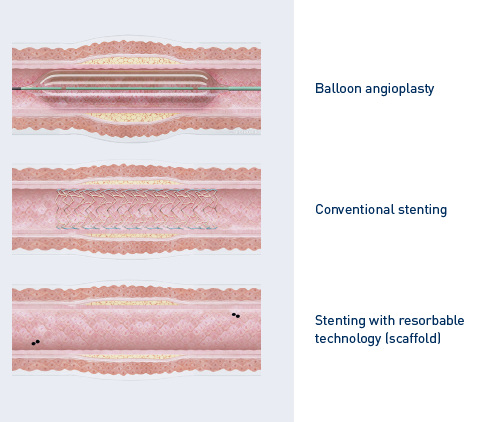
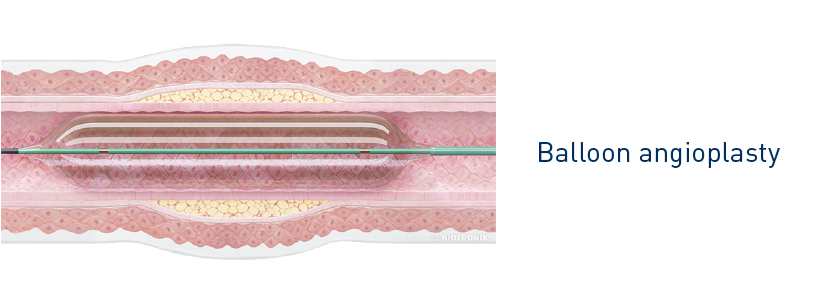
Balloon angioplasty
This procedure is performed with a special balloon catheter. A tiny balloon is mounted on top of this catheter. The cardiologist then directs the balloon catheter into the narrowing in the coronary artery where it is gently inflated.
As it expands, the balloon pushes the obstructing deposits against the vessel’s walls and widens the affected coronary artery. After deflating the balloon, the catheter is withdrawn from the body.
The blood can now flow unhindered through the coronary artery and supply the heart muscle with oxygen. After balloon angioplasty alone the chance of an acute re-narrowing is about 40%.1
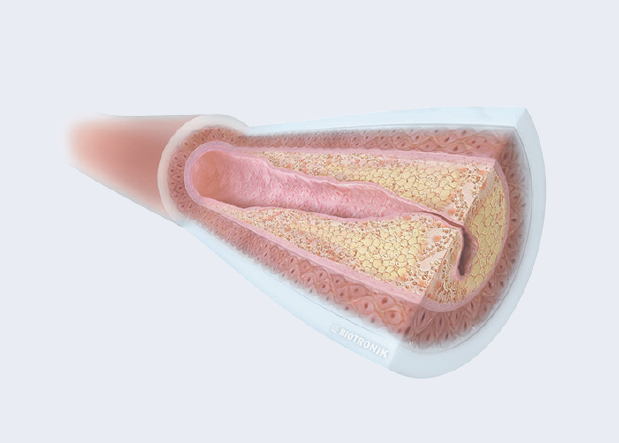
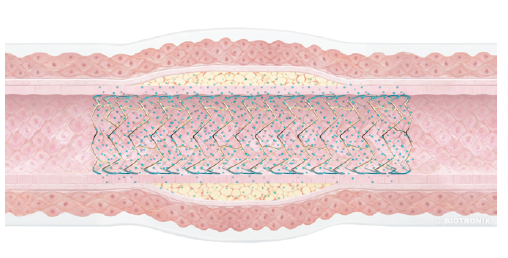
Stenting
Stenting is used to prevent an affected coronary artery from re-narrowing. A stent is a small metal mesh tube which acts as a permanent scaffold. The physician moves the stent (crimped on the balloon) to the affected site in the coronary artery via a balloon catheter.
At the target location, the balloon is inflated, thus expanding the stent which locks into place and forms a scaffold for the vessel wall.
After that, the balloon is deflated and removed, while the stent remains in the body, keeping the coronary artery open and allowing blood to flow freely again.
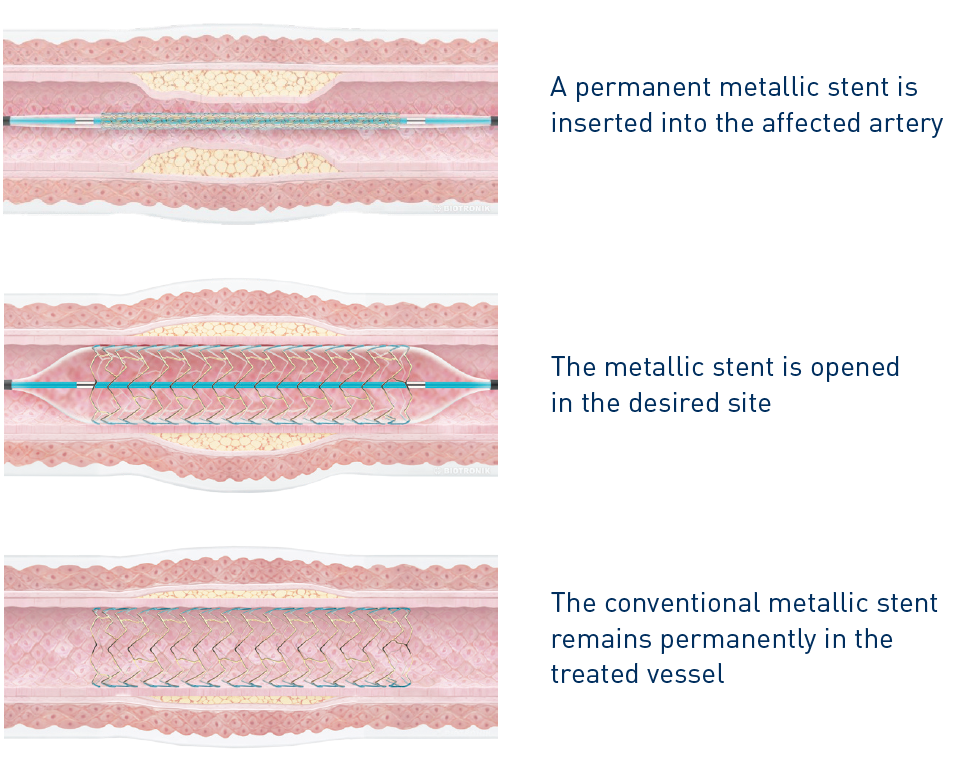
Drug-eluting stents (DES)
Drug-eluting stents, like Orsiro, are coated with a medicine which reduces the risk of the artery becoming narrow again after the angioplasty. The risk of a re-narrowing after DES-implantation is about 3-5% 2.
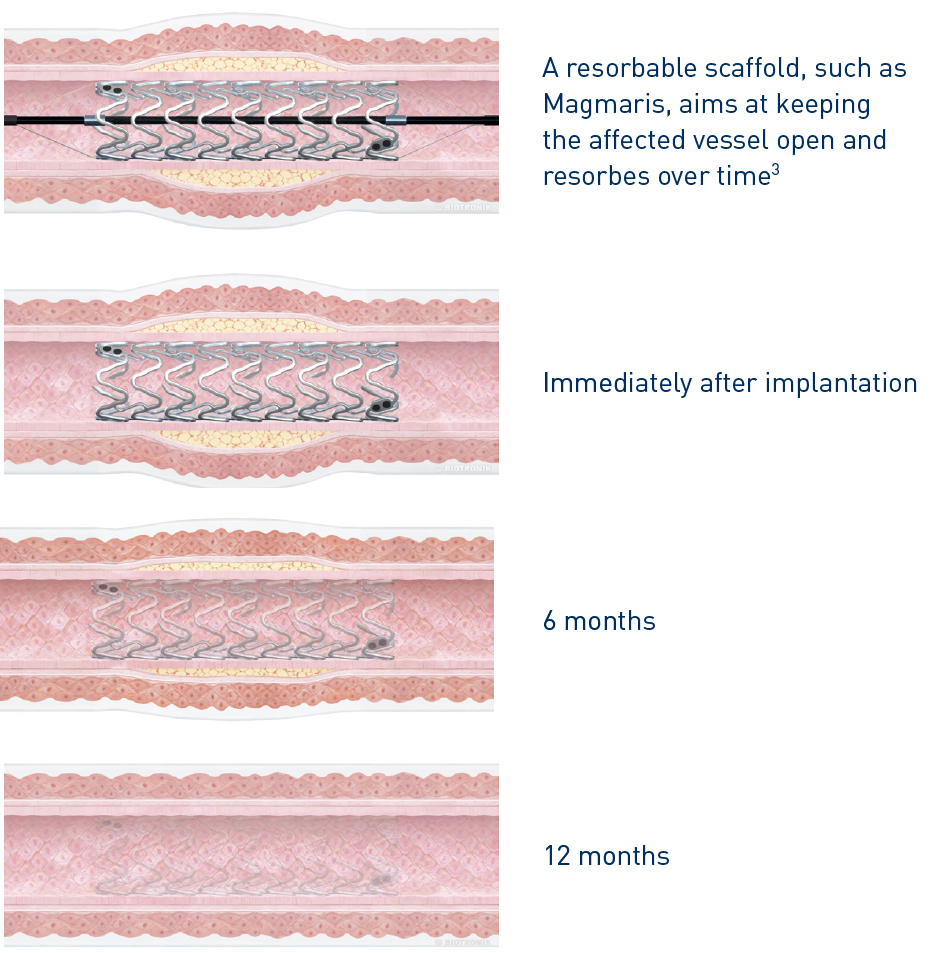
Resorbable scaffold
About 6-8 months after PCI the vessel wall is healed and doesn’t need the mechanical support of the metal-stent. Resorbable scaffolds (sometimes called bioresorbable stents) are innovative stents made of materials such as polymers or magnesium alloys that dissolve slowly over a period of 1-3 years.
As with a conventional stent a resorbable scaffold, like Magmaris, is implanted with the aim of keeping the affected artery open to improve blood flow. Resorbable scaffolds have the same medication to limit tissue growth and re-closing after the procedure as modern drug-eluting stents.
Unlike a conventional stent, a scaffold is not permanent and is resorbed over time. Once the scaffold is resorbed, it no longer interferes with natural vessel expansion and contraction.
The resorbable technology allows future interventions to take place without having to work around a permanent metallic implant.
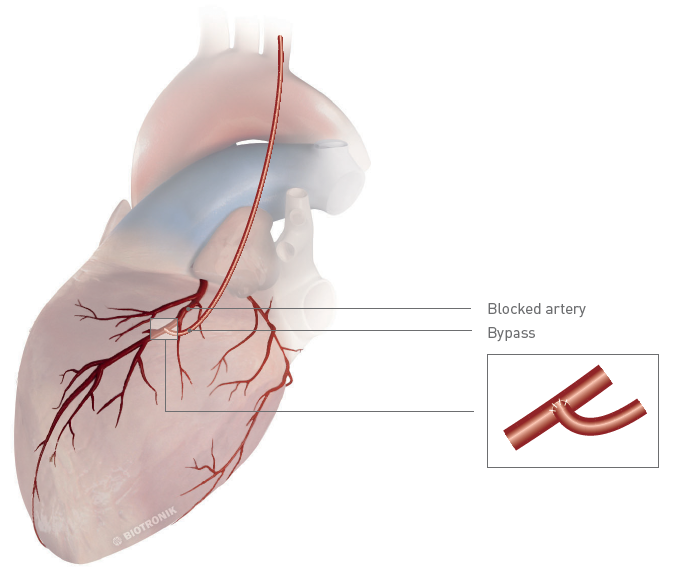
Bypass surgery
If a minimally invasive PCI is not possible, the patient will need to undergo open heart surgery under general anesthetic. A common type of heart surgery to help treat angina and CAD is called bypass surgery or coronary artery bypass graft (CABG). In this method, the blocked part of the coronary artery is bypassed with a segment of a healthy vessel secured from another part of the patient’s body. Blood can now flow around the blockage.
The surgery can be done while the heart is still beating (beating heart surgery) or while the heart is stopped and a heart–lung machine controls circulation (arrested heart surgery). Most patients with relevant CAD can be treated with PCI4, but there are limits. If for example the number of stenosis is too high or the location of the stenosis is too difficult, bypass surgery can be the better option.
Your doctor will recommend the most appropriate treatment (stent, scaffold or bypass-surgery) for you.
1 Alfonso F, Zueco J, Cequier A, et al. J Am Coll Cardiol. 2003;42:796–805.
2 SCAAR. Restenosis in stents 2007 to January 11th 2017 report. http://www.ucr.uu.se/swedeheart/images/stories/stent_reports/20170111/Bild4.gif
3 ~95% of Magnesium resorbed at 12 months. Joner M, Ruppelt P, Zumstein P, et al. EuroIntervention. 2018 Feb 20. doi: 10.4244/EIJ-D-17-00708.
4 Patel MR, Dehmer GJ, Hirshfeld JW, et al. J Am Coll Cardiol. 2009;53(6):530-553.

