Overview
Why would your patients need a comprehensive physiologic pacing?
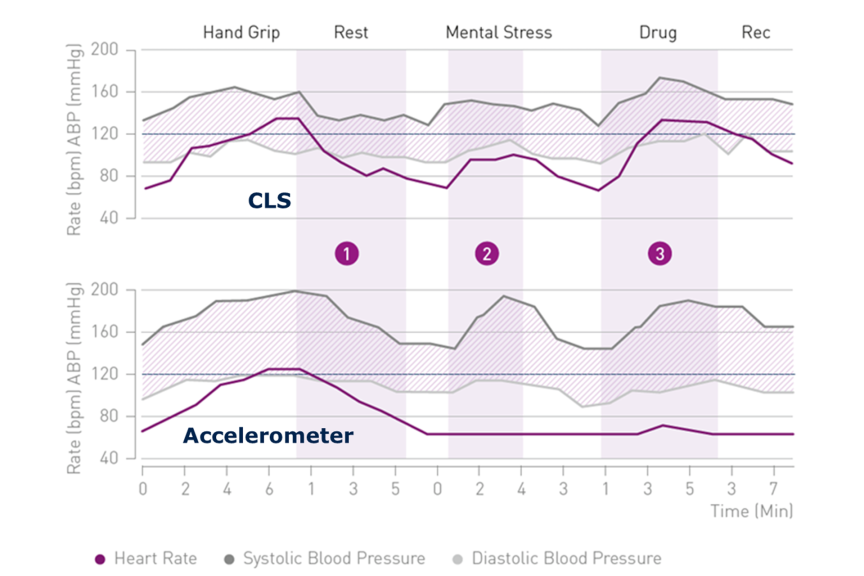
Every person experiences physical and emotional stress during their life. Regular daily activities, sport, or even playing chess or watching a video can result in such stress. If they suffer from chronotropic incompetence (CI), the patient's heart is not able to respond correctly to the stimulus. Studies have shown that CLS can improve the quality of life of CI patients as well as those suffering from vasovagal syncope.¹
Thanks to CLS rate adaptation, pacemaker patients are also supported during emotional stress.
Which patients can benefit from CLS?
CLS is beneficial for patients with Chronotropic Incompetence (CI) and Vasovagal Syncope (VS) as well as patients with Atrial Fibrillation (AF). For patients suffering from CI, the PROVIDE study showed that 75% of patients programmed with DDD-CLS experienced significant improvement compared to only 22% of patients programmed in DDDR.²
For patients burdened with paroxysmal or permanent atrial fibrillation (AF), cardiac output is also of utmost importance when AV synchrony is lost. CLS is able to support these patients through a steady, reliable and flexible algorithm. CLS has also been shown to reduce the burden for atrial tachycardia patients compared with other modes. In the BURDEN III trial, CLS showed a 16% risk reduction of the primary endpoint of time to first atrial high-rate episode of at least six minutes, stroke or TIA compared to accelerometer. That risk reduction to 23% for patients with no AV block and 27% for patients with no history of AF.
For patients suffering from VS, the recurrence of syncope significantly decreases with a CLS system. The randomized, placebo-controlled, double-blinded, multicenter BIOSync CLS study demonstrated a reduction of syncope recurrence rate after two years by 77% with CLS pacing versus placebo³.
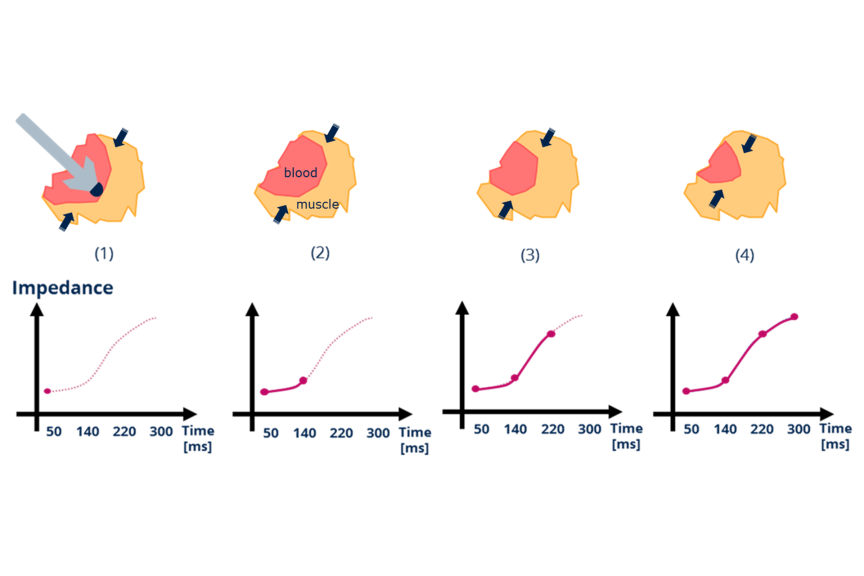
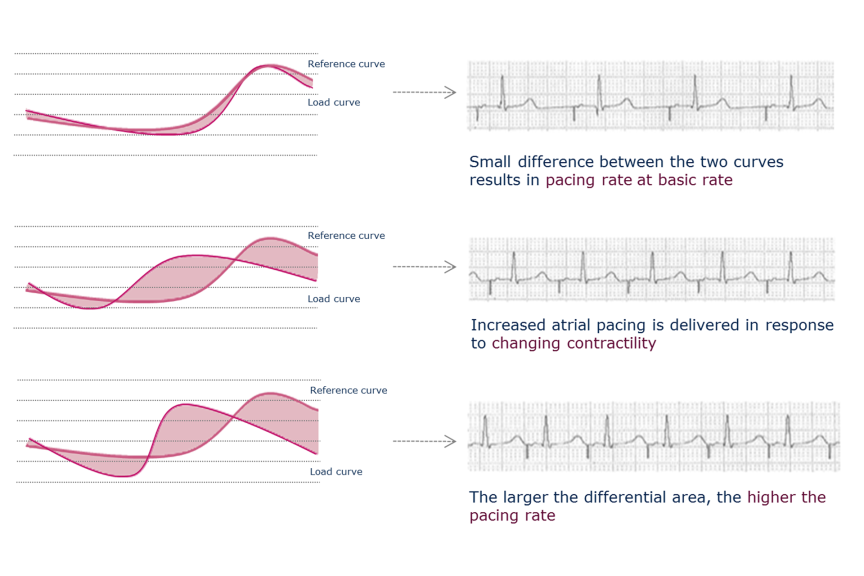
CLS continuously translates variations in myocardial contractility into physiologic pacing rate changes to appropriately support metabolic demands
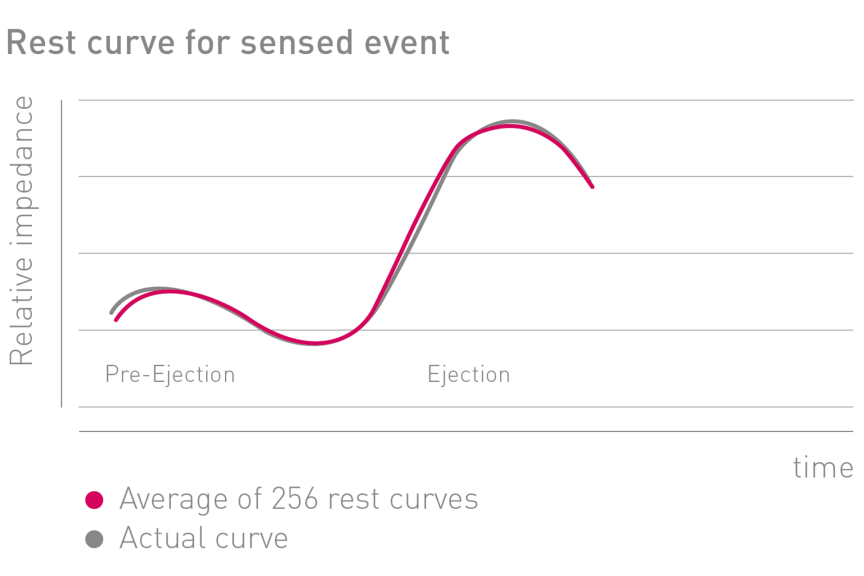
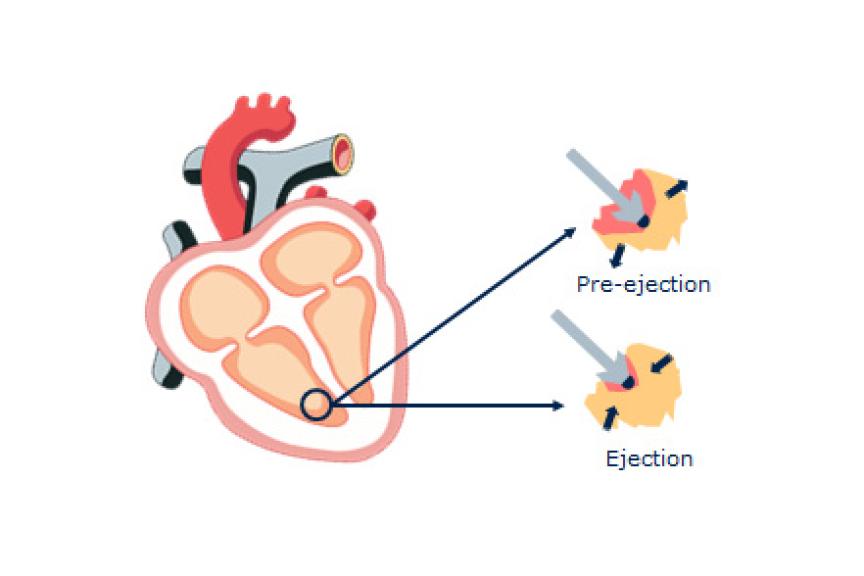
① Primary Sensor: Take measurements directly from myocardial tissue
② Built On A Beat-To-Beat Architecture: Rapidly evaluates every beat, and is able to respond on the next beat
③ Automated With Machine Learning: Learns the patient while automatically recalibrating to systemic variations (changes in medication, hydration, etc.)